To fully master your craft, you have to put the work in – and there is no such thing as overnight success. Harbir Sian chats with Dr. Julian Prosia, dry eye specialist and CEO/co-founder of Ophthalogix Canada, who emphasizes the need to spend “10,000 hours” to truly become a trusted expert in the medical field. He stresses the importance of continued education and collaboration for the optometric community to better serve their patients and communities. Dr. Julian also breaks down how to use amniotic membranes to treat dry eye and other related diseases while prioritizing accessibility and cost-effectiveness.
—
Watch the episode here
Listen to the podcast here
Putting In Your ‘10,000 HOURS’ To Become An Expert – Dr. Julian Prosia
Thank you so much for taking the time to join me here as always, guys. I’m always so grateful for all the support, liking, sharing, commenting, reviewing and everything that you do. It means so much to me. The show has been growing. Thanks to all of your support. As always, I have that big request off the top. If you get any value out of this, please do share it. Put up a screenshot. Tag us on Instagram or put up a link on LinkedIn. Let our colleague know that we’re having these valuable conversations that are going to help our profession to continue growing.
I want to say a big thank you before we get into our guests. A big thank you to the Canadian Association of Optometrists or the CAO, for giving us the space in Halifax at the conference center. We are here for the bi-annual congress. It’s an amazing show as always. The CAO does such a great job with this. A big thanks to CAO for giving me the space to record this episode. My man, Dr. Julian Prosia is the owner of Ophthalogix Canada. He graduated from Nova Southeastern in 2021. He is a big dry eye guy. If you follow him on social media, you’ll see all the amazing content that he puts out there @DoctorProsia.
You’ll see all the great content he puts out and you’ll see he’s a big into dry eye already. Early in his career, in 2021, he’s made such a huge impact in the dry eye space and optometry and bringing amniotic membranes, making them more accessible to us. Thanks for being here, Julian. I appreciate it.
It’s a pleasure to be here.
Dry Eye Specialist Dr. Julian Prosia
I’ve been excited to do this. We only got to know each other but I feel like we’ve become fast friends and got to know each other quite well in the last few months or so. It’s been good. If you don’t mind, tell us a little bit more about who you are and what you’re up to in the industry.
I practiced in Hamilton, Ontario. I practice about four or five days a week. It’s a pretty large dry eye practice. It’s pretty much what I love to do. It’s my passion. A little bit of primary care but a lot of dry eye. On the side, which has become a lot bigger now, was Ophthalogix Canada, which we founded in 2023 where we brought amniotic membranes to Canada, both Health Canada approved and FDA approved, which is exciting. As a dry eye guy, one of my favorite treatments is amnion because of the wow factor that gives patients. Now, I get to share that with all the amazing Canadian doctors, which is very valuable.
You’re passionate about it, which is cool. That’s palpable. When you were in Vancouver a month or so back, I could feel that. When we’re in the room and you’re talking about it. I’m like, “This guy is passionate about it.” It makes me as a person who’s listening, as another practitioner listening starts to get more interested.
What Is An Amniotic Membrane
We’re going to share that in a minute because it did get me interested in bringing amniotic membranes into our practices as well. Before we start diving into all the technicalities of Ophthalogix, amniotic membranes and patient experience and all that. For those of us who have less experience in this, what is an amniotic membrane? How or why does it work?
The technical term of what an amniotic memory is the innermost layer of the fetal placenta, the baby placenta. What they found in this placenta is that it has healing capabilities to heal, let’s say abrasions, anti-angiogenic properties like for neovascularization and anti-fibrotic for scarring. A wide array of different healing capabilities because essentially, like a stem cell can become any type of cell.
What we did is we were able to extract this and create almost like a little disk that can be placed on the eye for healing capabilities. Now, you’re seeing over the last two decades the use cases for amnion and placenta in general. It’s exploded nearly 10 to 20 times with almost 60% of it coming from North America, which is crazy. We haven’t even scratched the surface of what we can do with these things. For the eyes, it’s valuable because we can heal up to 32 different indications of the cornea.
We’re talking recurrent corneal erosions, improvement and reduced recurrences. We’re talking about sterile ulcers, persistent epithelial defects or your basic recalculation dry eye patient, which is what you’ll share with your patient. There’s a lot of different use cases where you don’t have to be a dry eye guru to be, “I need this in my practice. I don’t treat dry eyes.” You can use this on an emergency basis. You can do this for things that you are going to see on your day-to-day, which is nice. You don’t have to be in dry eye.
Everyone has good ideas, but what makes the difference is the implementation and the understanding of how to get started.
How did you get around to starting Ophthalogix? Why do you think that was needed?
I practiced for about two to three years in the states, and I had the pleasure of practicing alongside two ophthalmologists. I’m still keeping contact with them. They’re very great guys, but they showed me the path to a more medical basis of what Optometry is as a whole, which is valuable. We spend our dials. We get those patients in nice glasses and things like that but there’s a whole other side of the story that I was in love with. I wanted to make patients feel better.
The reason why I got into this is, I’ll share a little story of a patient of mine that I still keep in contact with. She was one of my patients. The first week that I got out of school, she came in complaining of severe dry eye problems. As a new grad, that’s daunting. You’re like, “What do I do for these patients?” I learned what I learned in school but I don’t necessarily have the experience. Believe it or not, it still gives me chills. She handed me a suicide note.
She told me that she just went through cancer therapy. She’s been struggling beyond belief and needed someone to help her. I did some diving into it. I read some corneal magazines and did my own research at home and figured out, “If I need to help her with pain, what is the number one thing that we can do to modulate pain?” That was an amniotic membrane. Thankfully, I was able to figure out Ophthalogix in the states. I was able to bring it in.
I did my first ever amniotic membrane on her and she is still alive now. She keeps in good contact with me. She nominated me as a top doctor in Boca Raton for 2023 and I won. To this day, I still keep that award that I got on my desk because it reminds me every day of why I got into this in the first place. It’s not about anything other than helping these patients. I feel that the amniotic membrane is so powerful that if I can do it and you can do it, we can help so many more people.
That’s a very powerful story and very moving. Again, your career is quite young still. That was only a couple of years ago and you have already achieved that. I should have mentioned that off the top, a top Doctor of Boca Raton in 2023. That’s a nice accolade to have but what a crazy story that led you to receive that honor.
That’s the story that’s going to stick with you forever, I imagine. That’s not something you’ll ever forget. That’s something I’ll remember now forever because it’s so profound. That’s amazing. That is what led you to dive more into amniotic membranes. What about starting the company? Tell me what goes into that like to start an actual company, the ins and out of that.
As eye doctors, we go to school to learn how to be doctors. We don’t learn the tangibles of how to start a business. At the beginning, especially when you’re trying to start something. We all have good ideas but to implement that into your day-to-day and to create an idea to form it into a business. It’s very difficult. There’s a science behind it. I brought in my brother, John Paul, which you obviously know. He has a business background and I basically laid it out on the table for him and I said, “I love helping people. I want other people to get this ability to help others. I want to extend this out to all my Canadian friends and Canadian doctors. How do we do this?”
He’s a young guy too, but he pushed me in the right direction. He put me into the places I need to be to maximize our ability to start this business. If it wasn’t for him, I wouldn’t have had that opportunity to create that. Everyone has good ideas but it’s all about the implementation of it, the tangibility of it and the understanding how to start that. A big shout out to him, for sure.
It’s a good point. Some of us, not myself included in this specific case. Some of our colleagues do have a knack for business. Maybe that’s just something when they were young, they were entrepreneurial or for whatever reason they have that ability to run businesses and understand numbers and how to bring things to market or grow their own business. Whether it’s an optometry clinic but others and myself included, do not have that knack. It’s nice that you have somebody in your family who has that.
I love seeing family businesses. I’ve seen that in multiple cases where the medical person has the medical idea but they’re brother or sister or wife or whoever has the know-how to bring that thing to market. That’s so cool. From an outside of my perspective, it makes it more engaging for me to know it’s two brothers. It’s a family business. It’s cool.
It’s that mom and pop shop feel. We know as optometrist, when you go into a private practice and you have that mom and pop feel. It’s like Susie down the street and her dad’s going to come to you. All of a sudden, it’s a big family. It is nice in terms of that side of industry getting that closeness and that relationship-based approach.
What’s interesting is, now having multiple conversations with you and with JP. I feel like I’m almost talking to the same person. There’s not a big divide between you’re the doctor and he’s the business guy. You guys both know so much about both sides of the business or all sides of the business. When I speak with JP, he’s talking about the technicalities of the amniotic membrane. I’m like, “That’s pretty cool. You know more than I do.” That’s good because he knows the ins and outs of the business. That’s great.
Collaborative Work Within The Optometric Community
The word industry is going to come up a lot through this conversation and I’m curious and share as much as you’re comfortable sharing. How did the industry accept you as a player of Ophthalogix as a player in this space? Theoretically, you’re a very niched product, but you will be potentially taking ground from somebody else who has some other dry eye product or corneal product that may be helping patients. Have you felt that or not? It’s so niche that it’s not stepping on anybody else’s toes.
I have to say the industry partners that I have had the pleasure of coming into contact with. I’m going to give a shout out to Thea and Sun Pharma. These are industry partners. They’re general focus is education. They want us to learn so that we can teach our patients. As a doctor, everyone on the outside thinks that as a doctor you know everything but we don’t. We have to be taught the tools and know our knowledge from school and our knowledge basis. We can use those tools to help our patients.
If you have a good industry partner who is willing to take the time to educate us in the proper way, then it just makes it easier. Everyone helps each child there. I felt that a lot of the industry partners that I had the pleasure of interacting with have been almost like an adjunct to our business. They’ve brought in so many different exposures across Canada. We’ve collaborated. When I was in the United States, I didn’t see that as much. That’s why I love being here in Canada. It’s the fact that there’s so much collaboration. There’s so much inter industry collaboration and it does help smaller businesses like myself or smaller businesses that are trying to start out become something bigger and get widespread exposure.
I love that a larger company organization like Sun or Thea would give you that support and see it as a collaborative effort versus competitive. That’s how I got to know you or saw you, at least in person, the first time. It was at Thea/Ophthalogix collaborative event in Vancouver. I love to see that collaboration and those companies, in my experience, in particular Thea. Those companies have been incredibly supportive of optometry, optometrist of the industry always with this growth mindset.
Dealing With Industry Challenges And Barriers
It’s nice that it’s been your experience as well. Let’s talk a little bit about that. You go to these dinners. You host these dinners, meetings, you talk and you do presentations and webinars. You talked to a lot of Optometrists. Amniotic membranes are fairly niche as we said and they feel very specialized. What concerns, barriers or hurdles do you think ODs are facing when looking at getting into this type of space?
That’s a good question because there’s this perception that it is extremely specialized and extremely difficult. It’s very accessible in other parts of North America. It’s very simple to do. It’s just we haven’t had the educational exposure of it and it goes back to what you were saying with the industry. If the industry is educating, then we have those players educating us to feel more comfortable in using their products.
I feel like that hasn’t been done well in Canada, in terms of educating about amniotic membranes. Even any biologic, to be frank. I don’t know why but, for me, it was a driving force to be like, “Absolutely not. We need this. It’s going to help our patients. I’m going to be the one to help educate everyone about it, so we can all work together.” That’s the main MO that I always operate with because at the end of the day, who’s our main focus?
Our patient. When we get a little caught up in our own thoughts, we bring it down to the patient. What is best for the patient? What are we doing that’s going to help this patient? You make your decisions from there. That’s our North Star, ultimately. How are we going to help our patients to serve them better? I will agree that it feels too complicated. The word and the term amniotic membrane. As soon as you say that, it triggers this feeling of like, “Too much for me.” I’m not that specialized. I’ll leave that to Claudine or somebody like that. That’s not my forte.
I’m going to share my experience in a minute but having done one now, I agree with you. We have way over complicated the process. It’s shockingly simple. Janice was coaching me through it a while back and she’s like, “Harbir, please just stop. Trust me. This is going to be easy.” Yes, I would agree. I’m going to share a little bit about that in a minute, but let me share what is another hurdle and I’d like to hear your thoughts and that’s cost because these are not cheap. Tell me what you’re hearing from ODs as far as our colleague and patient saying, “This is too expensive.”
The amniotic membranes are the most powerful punch you can pack in your office to make a patient better in a span of a few days or weeks.
In a lot of the things when it comes to specialty care, there’s a lot of problems related to cost. We don’t have the necessary coverage in my opinion we should have. If you compare it to something like IPL or radio frequency. Any of these large machines that cost upwards of hundreds of thousands of dollars, you’re investing in that as an upfront cost. You have to use that plenty of times for a patient to get better. Even though it does work, you will be paying that off for a while, unless you have the necessary means to buy cash, which not every doctor has.
The amniotic membrane is the upfront cost of about $485 to $489 and you can apply that knowing that the patient is ready to do it. We have doctors that will order on a case-by-case basis. They are making the returns 100% during that day that they receive it. We also have other doctors that will order in bulk and take advantage of the fact that even though it is a little more expensive, we’ll cut the cost of the doctor a little bit down.
Also, the fact that it lasts five years. You have the opportunity to invest in it with a couple of thousands of dollars to make back all of that, times 100%. Yet you’re not paying that $100,000 worth of investment into the IPL or whatever it is. Anything in that dry eye space, expense is always something we think about but if you compare it to the other big players in dry eye. It’s relatively inexpensive.
That’s a bit of a mindset shift that we need to make. We were trained. As business owners, we look at capital investment in this capital equipment. It’s normal. I got to go buy a retinal imaging or a camera or an OCT. Where it used to be like, “I got to put down the $50,000 or $100,000 and I’ll make it back over time.” Whereas, this is one of those things where it’s almost an immediate return on that.
From a business owner’s perspective, a little shift in my mindset might help me see that cost differently. What about from the patient perspective? Do you find that doctors are saying they’re patients are complaining about cost? Is it that most of these patients are in such a dire need that they’re like, “I’ll do it no matter what the cost is?”
We’ll talk about it and what an amniotic membrane is for the audience that doesn’t know that. The amniotic membrane, in my opinion, is the most powerful punch that you can pack in your office to make a patient better in a span of days to weeks. What do we have that’s tangible in our office that can do that? Maybe the closest thing is potentially a steroid. For things like ulcers, what can do that? Nothing.
These patients that are needing this, in dire need as you said. They’re willing to do anything just for comfort. These are the patients that need the help. Even though it is an expense, most people I find, even those patients that are on disability, are willing to invest in their own health so that they can get back to their day-to-day. Let’s call it $8,000 for your livelihood. There’s always going to be people that do not want to put that up.
That’s why also actively, I’m trying to get insurance coverage to underwrite the state side, which already has coverage for this. That’s another thing. Knowing that the United States already has this covered for almost 100% for a large variety of people. We’re not far behind. We just need to push for that. Push for us as doctors and push on behalf of the patient as well.
I want to give a quick tip of the cap to the CAO for always working on that. In an upcoming interview, I’m going to be recording with the president of the CAO. They’re working with insurance companies to try to get more coverage from insurance companies for increased reimbursements flat out just for eye exams, but for more technical stuff like this as well and a lot of its going to come down to. I know you’re doing all the good work there, but talk to your associations.
As they’re working with the government to increase reimbursements or scope or whatever it might be, to try to get some more of this stuff included in there. I’ll give an example with BCDO. They’ve done a good job in proving or increasing MSP, which is the equivalent of OHIP coverage for different things. For example, we now have a billing code for myopia management. It’s specific for certain types of patients or certain prescriptions, but that’s how it started.
As they see this code is not getting abused. It’s being used appropriately and there are a lot of kids that need it. We’ll increase the use of that. We have a code for scleral lens or hard contact lens fitting, specialty lens fitting for keratoconus, so unilateral or bilateral based on what the need is. It doesn’t cover the whole cost of the thing but it covers a chunk of it. Work with your association and the government to start to add some of these. It’s not that far-fetched to think we should have a code for amniotic membranes. This is a product or a medical device that’s going to help patients.

It’s like I said before, it’s not anything that we have to reinvent the wheel on. It’s more so the exposure like you’re saying, getting out there and getting people to understand why this is beneficial to our patients and why it is almost necessary in most cases. What we’ve developed on our end is, we developed a system where a doctor can take a template that we’ve provided to them. All they have to do is basically check off the ICD-10 code that’s already on the form that underwrites the US system.
The insurance companies will start to see this and say, “This doctor and this doctor are sending us these things. What is an amniotic membrane?” That’s how that conversation starts. We also have CAO behind us to make that initial push as well. As you said, it’s so important for us to get the word out for the next steps in eye care so that we can proceed and grow as an entire career.
Harbir’s Experience With Amniotic Membrane
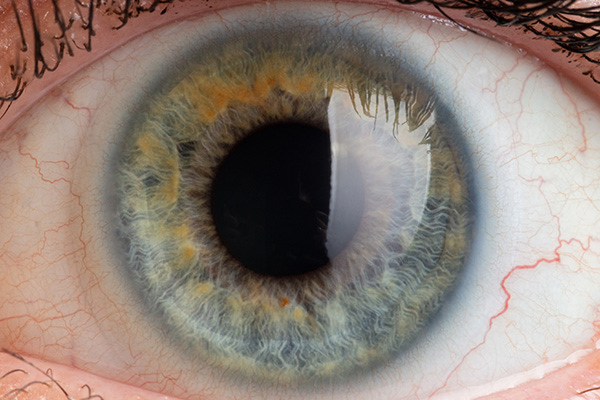
We’ve touched on it, it’s not that complicated. I said that I’ve had my own experience and I had to get coached through it. I wanted to quickly share what my experience was. I’m sharing this because I imagine there’s somebody else out there who’s watching or reading who’s like, “I’ve heard about amniotic membranes. It’s not for me, or I don’t have any patients that could benefit.” When Julian was presenting in Vancouver a couple of months ago, he was giving the case of a specific patient who had this recurrent keratitis or stubbornness. It just wasn’t going away.
The patient had some mixed connective tissue or autoimmune type condition that was likely connected to this somehow and showed images of the epithelial defects and the staining. I was like, “That looks like a picture of my patient’s eye. The patient history sounds like this patient I’ve been trying to help for months with everything. I’ve thrown everything at it.” It waxes and wanes. Some days, she’ll come in and be like, “It’s noticeably better,” but it was because we doused it with steroids, ointments and everything. It’s not something that we can maintain for a long period of time.
Anyways, I’m at your dinner talk and then I approach you after saying, “This is the patient.” The patient was at a point where I tried everything. I told her I tried everything, so now I was either going to put scleras on her or send her to maybe Manya or somebody else to try PRP then I saw you. I called the patient that next week and I said, “I have an opportunity for something different. Would you like to try this amniotic membrane?” She immediately said yes because she was a little hesitant about the whole scleral lens thing. I came in and then I talked to you multiple times. I’m texting you, Claudine and Janice. I’m like, “Help me out.”
I’m always available.
You have been. I even picked up a speculum. This thing took like a village was helping me here with this. I picked up a speculum from Evelyn’s office and didn’t end up needing the speculum, as you had told me. The patient did have pretty strong eyelids but she was very minimal and she was patient cranked over her eyelids. Using your reverse geometry forceps, place the amnion.
Yes, it does the thing where it curls but I flipped it because it’s double-sided. I was able to just flip it and it settled down. Almost like you put a piece of paper on a wet surface and then you smooth out the wrinkles. I didn’t do a great job of smoothing it out, but it stayed on. I put a bandage contact lens on. The whole actual process of placing amnion on was like 30 seconds.
It’s crazy to think it’s that easy. I always say keep it simple stupid because sometimes, we like to overcomplicate things. It’s not that hard.
It wasn’t. I made a video but I didn’t get patients approval to share it publicly, but I’m using it for staff training. She was okay with that, like showing other doctors. The doctors were like, “That’s it?” It was a one minute video and half of it was just me saying, “Are you ready,” and getting the right camera angle. The actual placement of the amnion was like 30 seconds and BCL, as we all do. BCL is for bandage contact lenses. It’s pretty easy. That was that.
She came back a week later and it was remarkable. The results of the pre and post, I posted on Instagram. You don’t see the patient’s face so she was okay with me posting that. Go to my Instagram, @HarbirSian.OD and you’ll see it there. I don’t post a lot of clinical stuff. It’s the only one that shows a picture of a cornea. It’s pretty easy to find, but you’ll see the pre and post. It’s remarkable. It was like a diffuse SPK that covered probably 75% of the cornea, deep staining prior and a week later, I would say 90% of that was gone.
Keep everything simple. Avoid overcomplicating things whenever you can.
It was just punctate little things around the cornea still but remarkably better. The patient felt much better when I saw her for a follow-up a few days later. I showed her the picture of the before and after. She was like, “Wow.” Even she was shocked because I’ve shown her pictures of her cornea before and I was like, “I don’t know what to do with this. It’s just not getting better.” It’s a remarkable result.
For me, it’s such a positive experience that I will now be looking out for when I can use an amniotic membrane because I know it works and it’s not that hard to do. If you’re reading and you think you may have a patient that could benefit and you’re on the fence. Reach out to Julian. They have videos on their website also, which I looked at. Again, I watched the videos and was like, “It can’t be that easy,” but it is as simple. Let’s not use the word easy. It requires some medical expertise and your ability to hold forceps in place and all of this stuff and knowledge of how to be around the eyeball in the cornea.
It’s a lot easier than removing a foreign body like if you’re digging in there with an algebrush or something like that. It’s not nearly as complicated as that. Anyways, I’ll stop with that, but I would encourage anybody out there. If you feel like you have a patient who could benefit from this, make sure you reach out. That’s just from my own personal experience. That was only a couple of weeks ago.
It’s shocking to see that you went from being like, “How would I do this? Where do I even start?” To, “That was pretty easy and my patient feels better.” That’s our entire goal not just as a company but also for myself. I want to instill that confidence in doctors where you could have twenty years of experience, one year of experience or three years of experience. It doesn’t matter who it is or how you practice. I want you to have the ability to say, “I have a patient that needs something like this and I don’t need to send this patient three hours up North to get it done. I can make this patient happy.”
At the end of the day, we know that regardless and despite everything else in life, especially in your practice. If you make someone happy, they’re either going to be part of your family for the rest of your life, a friend for the rest of your life or a patient for the rest of your life. It’s knowing that you have the opportunity to do it and it’s easier. Not super easy but easier for you to dive in and learn with all this exclusive and intensive training that you can help someone.
It’s much more accessible than I thought it would be. Approachable and accessible as far as getting the lenses from you guys. You ship them very quickly but also, the use of it is very approachable for any OD who’s used forceps, honestly, and has removed a foreign body. You’re very capable and you have the skill set to do it. Look into it. I’m excited that I got to share that with everybody because it was such a positive experience.
Application Of The TFOS DEWS III Treatment
Let’s talk a little bit more about medical dry eye type stuff. You’re deep in dry eye. There’s a DEUCE three report that’s just come out. Give us some highlights of that, if you don’t mind. I imagine you’ve gone through it and let’s talk a little bit about the application of what we’ve learned in DEUCE three to how we treat dry eye in the clinic. What are we doing right? What are you, in your perspective, are we missing perhaps based on the recommendations from the experts in the field?
DEUCE three does a great job of overlaying and summarizing everything that we know and should know about dry eye. In the grand scheme of things, we already knew this stuff. This is like a good review. There’s a lot of things that are already coming out or in the pipeline that we’re not included in the DEUCE three study. In that dry eye space, if you’re very immersed in it, you’ll see what’s on the horizon. DEUCE three did a great job of summarizing everything. It basically reinforced what we know.
The one thing that it didn’t necessarily highlight is give us a good roadmap to how to approach a patient. What you said, going back to understanding how to approach a patient. There’s a lot of gaps in my knowledge. I’m talking about the average patient or the average student coming out of school. I guarantee you. If you ask 9 out of 10 students, they’ll say, “I have no idea how to approach this dry eye patient.”
There needs to be more emphasis on case related studies, approaches, how to approach a dry eye patient in a combination way because we know. DEUCE three said it, “It’s a chronic inflammatory problem that is multifaceted.” There’s no silver bullet. We need to put more emphasis on teaching our students what dry eye is, the path of physiology and how to approach it. I don’t think DEUCE three touches on that.
Are you suggesting that there needs to be an algorithm or protocol for how to start treating certain patients? That would be nice to have but also, I imagine it would be quite varied from patient to patient because they’re symptoms and the process of the disease will be different for each person.
You look at a book like Malcolm Gladwell’s Outliers. 10,000 hours to become a professional. Experience is going to make you better at what you do but I’m talking more along the lines of giving these newer learners in eye dry almost like a road map, like how do we approach this patient? Not just use IPL or radio frequency on every single patient.
It’s diving into, what is this patient struggling with? What’s the path of physiology? Do they have any underlying comorbidities? How are we going to approach this? Every patient’s like a fingerprint. You’re never going to have the exact same case. If you treat it that way, you’re not likely to have a very successful outcome. It’s not as simple as a copy and paste. We all know that in dry eye because it’s such a difficult thing to treat.
There’s a lot of emphasis on evaporative dry eye, technology and treatment modalities that are aimed at that. Do you feel like aqueous is more prevalent than we think it is or less? Are we missing some obvious treatments on that side of things? For example, I don’t punctual plugs ever, to be honest. I would be part of the problem.
If you’re telling me that we’re not doing enough punctual plugs, I’m part of the problem but other treatments like the immunomodulators and things like multi-factorial disease. We have to target it from all these different directions. There’s been a big push in the industry to bring in devices that target the meibomian glands and fair enough, they may have some effectiveness. Did we get pushed a little too far in one direction? Are we missing something? Do you feel like where we’re at, generally speaking, we’re in a good balance?
I’m going to leave you with the stats. The average stat that we see of people that are diagnosed with dry eye disease is about 24 to 26 million Americans. They expect that that number is doubled to tripled because of the misdiagnosis or underdiagnosis of the condition. Whether that’s the patient not going or maybe the doctor overlooking and saying, “You’re fine. Use some eye drops.” Which we see pretty frequently.
If you apply that number and you extrapolate, then you say 24 million Americans and you multiply that by three. Fifty percent of those patients will be evaporative. That’s a stat. There’s not a lot of aqueous deficiency. They’re around 15% to 20% but only 50% is evaporative. That’s excluding mixed and aqueous. If we just focus on meibomian glands treatments or lid base disease, you’re only covering 50% of the 50% that are diagnosed.
If you were to tell me that stat that, “I’m going to treat you and we’re going to get 50% of the disease.” Does that sound good? It’s not necessarily aqueous deficiency in itself if we need to treat that more frequently. There’s so much mixed disease that I think one of the latest studies showed that mixed is almost rivaling evaporative.
Knowing that, why are we missing the other side of the story? There’s obviously great tools like IPL. Plasma pens are becoming good and lid based thermal pulsation-based treatments, but we leave the aqueous sufficient treatments in the dust mainly because of the prevalence of it. We’re forgetting about the whole mixed access.
The strictly aqueous deficiency is not very common or it’s much less common but the mixed aqueous evaporative combo is more common than maybe we’re giving it the credit for. It’s probably close to almost 50%. I would have underestimated that. I wouldn’t have thought it was that much but it could be those patients that I’m thinking of as just evaporative. They are evaporative but also they have an aqueous component that I’m not seeing or not treating or not approaching comprehensively.
It also depends on when you graduated, too. If you look back like, let’s say fifteen years. They would have told you that 75% of patients had the evaporative component. Now, we’re slightly scaling back. I think another report said 60% and now we’re down to almost 50%. We’re starting to understand that there is a hugely mixed component. In order to be super successful in making these patients happy and treating the disease, we not only have to address the one side, the lid disease but we have to put emphasis on whether that’s tear film inflammation or corneal problems. We can’t forget about those things. It’s the other half.
I had a guest on, Dr. Petar Prpic, who’s a contact lens specialist or special contact lens guy. A great guy and he said something. It was something that was told to him by a mentor or someone in the past and stuck with me. I feel like I want to keep sharing it because it’s something that is important for us to keep in mind. We’ve gone through a little bit of an era here in Vancouver but I think across Canada or maybe North America, where the use of certain devices has exponentially grown. People are acquiring these machines and using them in their office. Perhaps, there’s truly benefit to those RF, or IPLs or plasma pen or whatever it might be.
If medical tools improve due to technology, patients do not necessarily get treated better. The people using them must be highly capable as well.
I’m not knocking anything in particular. I’m just saying the acquisition of these devices and the use of these devices proliferated. There’s a bit of a misunderstanding of just because I have a device in my office doesn’t make me an expert in this space. I don’t want to make anyone upset about this. You may truly be an expert. I don’t consider myself an actual dry eye expert. I consider myself to have a certain level of expertise in it, but not an expert.
What Petar said about contact lenses was similar. Only because the eye fits the scleral, doesn’t make me an expert. An expert is the 10,000 hours you alluded to. An expert is somebody who looks at and this is what Petar shared with me, too. It’s like, just being able to do a thing, having a skill doesn’t make you an expert. Knowing when to use it or when not to use it or which aspect of that skill set to use, which tool in your tool bag. That’s what makes you the expert.
I’m not accusing anybody out there of not being an expert, but I hope that sinks in a little bit. We do dry eye, that’s great but to become an expert at it or to feel like an expert at it, I need to know when to apply IPL or RF or plasma or when not to or when to do a punctual plug or use a scleral or xiidra or when not to or an amnion, in this case. I thought that was important. Petar just shared that. It still resonates with me. It’s fairly fresh, but that applies to this. When is it mixed? When is it aqueous? When is it evaporative? Which tools do I use for all of those?
It’s not a multiple-choice answer in your room. If someone comes in, you look at the eye. It’s not, “This patient presents with X, Y, and Z.” You get to choose between four things like board exams. You’re looking at a patient and it is so much more complex. Even though you have the tools, knowing when to employ it. The analogy I always use is, you could have the nicest Porsche ever and you’re going to the Nürburgring and you want to get the fastest lap time. The guy in the Volkswagen who is a professional driver, will beat the Porsche. It’s all about understanding when to employ and how to do it.
As an optometrist, as a business owner, as someone that has a passion for our space in Optometry, I want to change that. I want to actively make and give people a roadmap to say, “You’re right, I do have an IPL. I do have this in my office. I do have amniotic members in my office but I’m not seeing the success rates that I want to see.” I want to change that. I want to make it accessible.
We talk about this all the time. We have such a good community of doctors out there like Claudine and all these people that are just as passionate as you and I about this. That coming together as a community to give access so that we can learn that road map so we can get all of the 48 million Americans or however many there are to get better. You think about it and you think back to 30 years ago when we had essentially no tools for dry eye. If the tools improved and things increased and the technology got better. Shouldn’t that mean that the patients are getting treated even better? Not necessarily. It’s just tools and toolboxes, but you got to be a carpenter.
Become An Expert Through Your Mistakes
I appreciate that. Julian, is there anything that you wanted to cover that we didn’t cover in this conversation yet?
If you’re a new grout out there and you’re reading. You will never ever on your first day of work know exactly what to do, but it’s not about that. It’s about having the wherewithal, the confidence and learning how to instill confidence in yourself to get back out there the next day and learn from that case that you may have made a mistake on. I’ll be the first one to say I’m not perfect. I’ve made so many mistakes, but did that shape me to be the person I am now? We got to learn from that and that’s how we become experts in the field.
Get In Touch With Dr. Julian
I appreciate you sharing that. Thanks for all the insight. Where can people find you, if they want to learn more about you personally and then Ophthalogix?
You can find me at @DoctorProsia on Instagram, @DrJulianProsia on TikTok but also just reaching out to me via email or dropping a DM if you want to learn more, not just about amniotic membranes but also if you want to shoot a case my way and get my opinion. I’m always happy to help and give back to the students out there.
I love that. Follow Julian on social media and get in touch. He’s very approachable, as you can tell. He’s a super nice guy but also very responsive. If you reach out to him with anything, he’ll be sure to get back to you. Thanks again, man. I appreciate everything. Thank you to CAO again for giving us the space here in Halifax at the convention center during the conference. I’m grateful to CAO for everything that they do to help support the profession to help us grow and for giving me this space here. Thank you to everybody who’s reading and watching the 20/20 show. Canada’s number one Optometry show.
Important Links
- Dr. Julian Prosia on LinkedIn
- Dr. Julian Prosia on Instagram
- Dr. Julian Prosia on TikTok
- Ophthalogix Canada
- Canadian Association of Optometrists
- Thea
- Sun Pharma
- BCDO
- @HarbirSian.OD on Instagram
- Outliers
About Dr. Julian Prosia

Dry Eye Specialist
CEO & Co-Founder, Ophthalogix Canada
Doctor of Optometry, Mountain Eye Care
Dr. Julian Prosia is an accomplished Optometrist and nationally recognized Dry Eye Specialist, currently practicing at Mountain Eye Care in Hamilton, Ontario. He is also the CEO and Co-Founder of Ophthalogix Canada, a rapidly growing eye care innovation network partnering with Canadian optometry schools, major hospitals, buying groups, and over 100 private practices nationwide.
Born and raised in Ancaster, Ontario, Dr. Prosia earned his Honours B.Sc. in Biology from McMaster University in 2017. He continued his education at Nova Southeastern University in Fort Lauderdale, Florida, where he completed a second Honours B.Sc. in Vision Science (2019) and graduated as a Doctor of Optometry with Highest Honours in 2021.
Dr. Prosia brings a wealth of experience from his time in the United States, where he served as a partner at a leading MD/OD joint Dry Eye and Cataract specialty practice in Boca Raton, Florida. During his 2.5 years there, he worked closely with the largest rheumatology practice in the region, co-managing over 6,000 autoimmune-mediated dry eye patients.
He has performed over 2,500 Amniotic Membrane Therapy procedures, making him a top provider in Florida, and has managed over 50,000 patients suffering from Dry Eye and Ocular Surface Disease. His expertise earned him the City of Boca Raton’s Top Doctor Award in 2022.
Dr. Prosia also served as the official eye doctor for the UFC Fighters Association, where he was responsible for triaging post-fight ocular trauma and determining fighter eligibility.
Now back in Canada, he has established a cutting-edge Dry Eye Clinic at Mountain Eye Care in affiliation with the McMaster Rheumatology Department and the McMaster Sjögren’s Clinic.
As a recognized Key Opinion Leader, Speaker, and Advisory Member for Sun Pharmaceuticals Canada, Dr. Prosia continues to contribute to the advancement of ocular surface disease management across North America.